The Centers for Medicare and Medicaid Services (CMS) announced two changes to regulations covering the additional documentation request (ADR) process for Medicare providers (except suppliers and physicians) under the CMS Recovery Audit Program.
Beginning April 15, CMS Recovery Audit Contractors (RACs) may request up to 20 records per 45 days from providers whose calculated limit is 19 additional documentation requests or less. Currently contractors may request up to 35 records.
Also, RACs will still be allowed to request additional documentation on up to 2 percent of claims, but of that 2 percent only three-quarters can come from any particular claim type, among them:
- Acute hospital inpatient (IPPS) claims
- Hospital outpatient (OPPS) claims
- Skilled nursing facility (SNF) claims
- Inpatient rehabilitation facility (IRF) claims
- Inpatient psychiatric facility (IPF) claims
- Ambulatory surgery center (ASC) claims
- Physician claims
The current regulations allows RAC auditors to make 100 percent of its ADR from any one claim type.
The number of ADRs is based on a provider’s Medicare claim volume from the previous year. The 2012 numbers that set the ADR levels beginning April 15 will be released on that date.
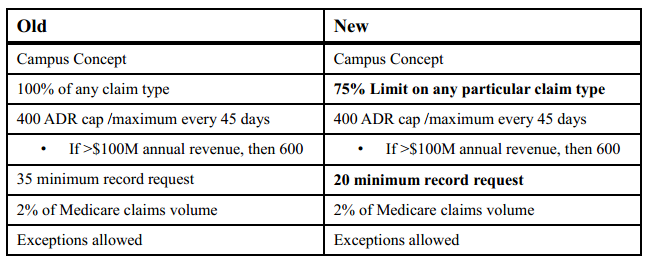
The chart below lists what processes have changed and what will change on April 15:




![[Image by creator from ]](/media/images/2015-04-cpf-report-training-key-component-of-s.max-80x80_F7Jisej.png)


![[Image by creator from ]](/media/images/Finvi_Tech_Trends_Whitepaper.max-80x80.png)
![[Image by creator from ]](/media/images/Collections_Staffing_Full_Cover_Thumbnail.max-80x80.jpg)
![Report cover reads One Conversation Multiple Channels AI-powered Multichannel Outreach from Skit.ai [Image by creator from ]](/media/images/Skit.ai_Landing_Page__Whitepaper_.max-80x80.png)
![Report cover reads Bad Debt Rising New ebook Finvi [Image by creator from ]](/media/images/Finvi_Bad_Debt_Rising_WP.max-80x80.png)
![Report cover reads Seizing the Opportunity in Uncertain Times: The Third-Party Collections Industry in 2023 by TransUnion, prepared by datos insights [Image by creator from ]](/media/images/TU_Survey_Report_12-23_Cover.max-80x80.png)
![[Image by creator from ]](/media/images/Skit_Banner_.max-80x80.jpg)